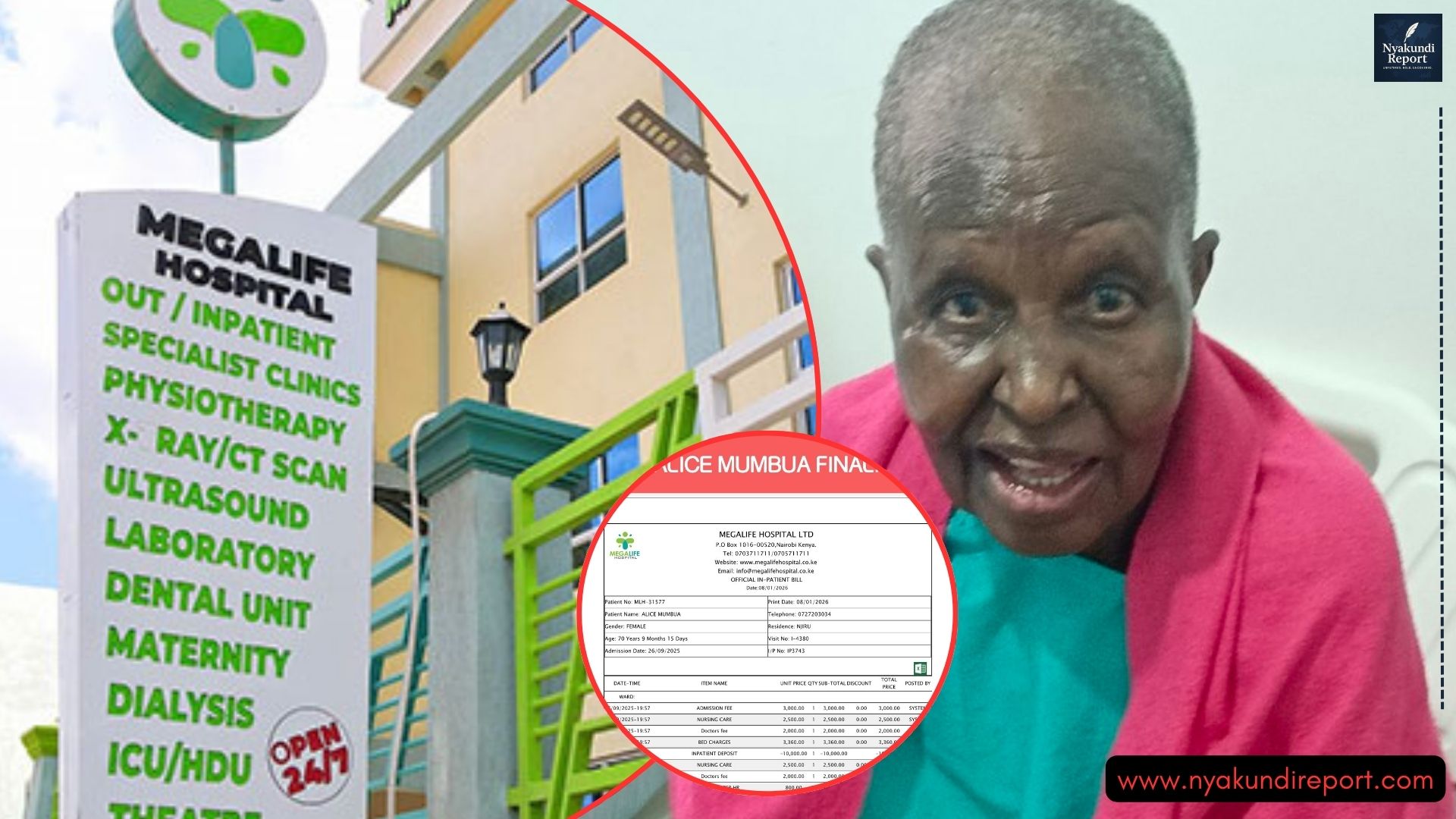
In recent months, the government has shut down 773 health facilities and downgraded more than 300 others. The move has raised concerns among Kenyans who rely on private and public health centers for care.
Many are asking what process determines which facilities are closed and which remain open. Understanding how health facilities are closed in Kenya helps the public know why accountability matters.

How Health Facilities Are Closed in Kenya
The process begins right from the registration of a health facility. When an applicant wants to start a clinic or hospital, they must first select a suitable location, set up the structure, and outline the services they plan to offer.
Once the application is submitted, the county government conducts a sanitation inspection. This inspection checks whether the facility meets public health and waste management standards. If the sanitation report is favorable, the applicant submits it to the Kenya Medical Practitioners and Dentists Council (KMPDC).
The KMPDC then sends trained medical inspectors to assess the facility. They check infrastructure, available services, and the equipment in place. Based on these checks, the facility is categorized according to the services it can provide.
If a facility meets all requirements, it is licensed to operate. However, this licence comes with strict conditions that must be maintained throughout the year.
Why Facilities Fail Inspections
Many facilities fail after the initial approval because they misuse the system. According to PS Oluga, some owners pass the inspection process but later move the licensed equipment to open another branch. This leaves the first facility under-equipped and unable to meet required standards.
One year after licensing, inspectors may return only to find that what was initially documented is no longer in place. Beds, machines, or even registered staff may have been relocated. In such cases, the licence is revoked, and the facility is shut down.
Fraud is another common reason for closure. Some facilities inflate patient numbers, claim for services not offered, or falsify treatment records. These fraudulent activities expose them to investigations under the Social Health Insurance Act.
Legal Steps Taken Before Closure
When fraud or non-compliance is confirmed, the Ministry of Health follows strict legal procedures. The regulator collects data, prepares reports, and submits the findings for gazettement. Once gazetted, the facility is officially marked for closure.
If fraud is serious, the matter is forwarded to the Directorate of Criminal Investigations (DCI). Prosecution may follow, with individuals held accountable for theft of public funds or misrepresentation.
PS Oluga stressed that these measures are not just about closing doors but protecting patients and taxpayers. By enforcing accountability, the government prevents loss of public money and shields citizens from unsafe health services.
He also pointed out that dishonesty is a bigger societal problem, and health facilities often mirror this culture. However, through cooperation between regulators and the public, stronger accountability can be achieved.
Conclusion
The closure of health facilities in Kenya is not random. It follows a clear, multi-step process involving registration, inspection, licensing, and compliance monitoring. While many facilities meet the requirements during registration, misuse of equipment, fraud, and poor service delivery eventually lead to shutdowns.
With over 773 facilities already closed, the government insists that the strict measures are necessary to protect patients and restore trust in healthcare. Understanding how health facilities are closed in Kenya highlights the importance of honesty, accountability, and continuous compliance with health standards.