SHA fraud claims probe reveals Ksh.5.1B under review.
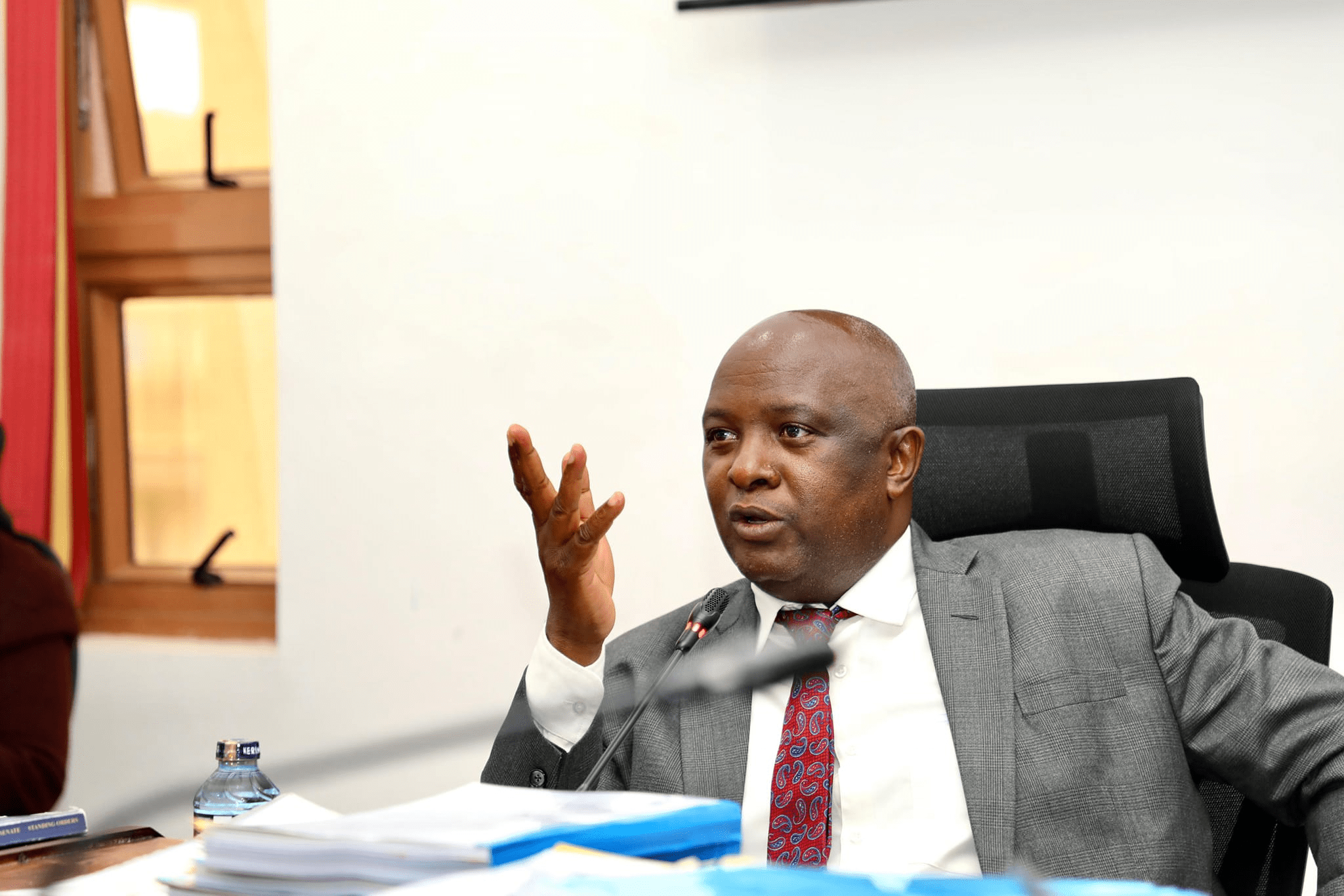
Health Cabinet Secretary Aden Duale says claims worth Ksh. 5.1 billion filed under the Social Health Authority (SHA) are now under review.
The government is conducting a crackdown to prevent fake billing by healthcare facilities.

Since TaifaCare began in October last year, hospitals have sent claims totaling Ksh.91.7 billion under the Primary Health Care (PHC) and Social Health Insurance Fund (SHIF) schemes.
Out of this, Ksh.60.7 billion has already been paid, while Ksh.6.4 billion has been approved and is waiting to be released.
Duale explained that not every claim is genuine.
He said Ksh. 3 billion worth of claims are being rechecked because they lack proper documents. Another Ksh. 2.1 billion is under close watch for possible fraud.
The ministry has also thrown out claims worth Ksh.10.6 billion.
These were linked to fraud such as false medical records, changing outpatient cases into inpatient admissions, and even billing for patients who never existed.
Recent audits revealed shocking malpractice.
At Nabuala Hospital in Bungoma, investigators found fake maternity claims, including multiple caesarean sections on the same patient within just a few days.
Kotiende Medical Centre in Homa Bay was also flagged for presenting fake clinical records signed by one person across both day and night shifts.
“These actions break Section 48(5) of the Social Health Insurance Act, 2023, which sets penalties for health providers who falsify information to cheat the Authority,” Duale warned.
According to SHA data, hospitals submitted Ksh. 9 billion in PHC claims, out of which Ksh. 7.7 billion has been paid.
For SHIF, Ksh. 82.7 billion in claims were made, with Ksh. 53 billion already disbursed. Claims worth Ksh. 7.6 billion from August is still under review.
The SHA fraud claims probe shows the government’s firm stance against corruption in health care and its push to protect taxpayer money.