Kenya is set to lead HIV prevention efforts in Africa with the rollout of the injectable HIV vaccine in January 2026. The new long-acting drug, Lenacapavir, will be available in public hospitals for free, especially targeting vulnerable groups.
This initiative positions Kenya among the first nine countries worldwide to introduce the twice-yearly HIV preventive injection.
The National AIDS and STI Control Programme (NASCOP) is working closely with international partners to ensure that hospitals across the country are ready for a smooth and equitable distribution of the new HIV prevention drug.

Initial Rollout Facilities for Injectable HIV Vaccine
Health officials have revealed that the initial distribution of Lenacapavir will focus on major referral hospitals and county-level facilities with existing HIV prevention programmes.
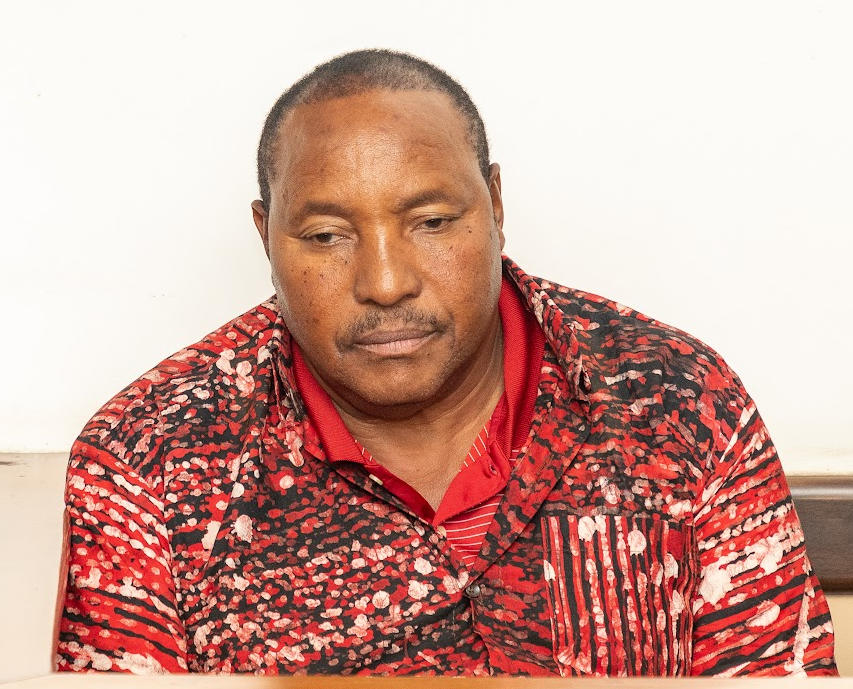
Although the Ministry of Health has not released an official list, NASCOP head Dr. Andrew Mulwa confirmed that the rollout will begin at public hospitals with the infrastructure and capacity to handle the new injection.
Major Public Hospitals Leading the Initiative
The rollout of the injectable HIV vaccine will begin in leading public referral hospitals, including:
Kenyatta National Hospital, Nairobi
Moi Teaching and Referral Hospital, Eldoret
Jaramogi Oginga Odinga Teaching and Referral Hospital, Kisumu
These hospitals have been selected for their extensive experience in HIV care and their capacity to manage large-scale preventive programs.
County-Level and Regional Hospitals Receiving the Drug
The government plans to extend the rollout of Lenacapavir to county and regional hospitals. Facilities expected to receive the injectable HIV vaccine include:
Coast General Teaching and Referral Hospital
Embu Level 5 Hospital
Kisii Teaching and Referral Hospital
Kakamega County General Hospital
Nakuru Level 5 Hospital
Garissa County Referral Hospital
Meru Teaching and Referral Hospital
Machakos Level 5 Hospital
Kisumu County Referral Hospital
Bungoma County Referral Hospital
These hospitals will provide critical access to populations outside major urban centers, ensuring equitable distribution of the HIV prevention drug.
Cost and Access in Public and Private Hospitals
Kenyans accessing the injectable HIV vaccine in public hospitals will receive the drug free of charge. Dr. Mulwa emphasized that affordability is a key priority to ensure equitable access.
Private hospitals, however, may introduce fees depending on their pricing models. Discussions are ongoing to balance accessibility, sustainability, and supply to ensure the drug reaches all eligible Kenyans.
How the Injectable HIV Vaccine Works
Lenacapavir is administered under the skin of the abdomen as a long-acting pre-exposure prophylaxis (PrEP). Patients typically start with oral Lenacapavir tablets to prepare the body for the injection.
Two initiation methods are available: the Day 1–2 method or a 3-day method followed by an injection after two weeks. Once fully initiated, the injection is given every six months, providing a convenient alternative to daily oral PrEP pills.
Health officials believe that Lenacapavir’s biannual dosing could improve adherence and reduce new infections, particularly among young people and high-risk populations. WHO guidelines now recommend long-acting injectable PrEP as part of comprehensive HIV prevention strategies.
Kenya’s HIV prevalence stands at 3.7%, with an estimated 1.4 million people living with the virus and 41% of new infections occurring in people below 24 years.
The Importance of Lenacapavir for HIV Prevention
The introduction of Lenacapavir marks a major milestone in Kenya’s fight against HIV. The drug’s long-acting formulation provides a discreet, sustainable, and highly effective preventive option. Officials hope it will reduce barriers associated with daily oral PrEP, such as adherence challenges and stigma.
Health Cabinet Secretary Aden Duale highlighted that Kenya’s participation in the global rollout reflects its commitment to expanding access to innovative prevention tools.
Lenacapavir is part of a broader international strategy involving countries like Eswatini, Lesotho, Mozambique, Nigeria, South Africa, Uganda, Zambia, and Zimbabwe. Its FDA approval in June 2025 has positioned Kenya at the forefront of preventive HIV care in the region.
The government is confident that the rollout will reach both urban and rural populations, ensuring equitable access. Public hospitals will play a critical role in providing free injections to vulnerable groups, while private hospitals will complement distribution to increase overall coverage.
By rolling out Lenacapavir, Kenya is taking a decisive step toward ending AIDS as a public health threat. The initiative promises to make HIV prevention more accessible, convenient, and effective, empowering citizens to take control of their health while reducing new infections across the country.